What is Postpartum Prolapse! Ever wondered why some women feel pelvic pressure or a bulge after giving birth? This could be due to postpartum prolapse, a common but often overlooked condition. What is postpartum prolapse, and how can women deal with it? Here are the top 5 key facts about postpartum prolapse.
Pelvic organ prolapse is when pelvic organs (like the vagina or bladder) fall from their normal place due to a weak pelvic floor.1 Postpartum prolapse, as the name suggests, happens after birth. It affects 30-50% women and is a result of pregnancy and childbirth’s physical strain.
Postpartum prolapse can cause issues like pelvic pressure, trouble urinating or having a bowel movement, and pain during sex.1 It is treatable with non-surgical methods such as pelvic exercises or surgery if needed. To avoid or manage it, staying a healthy weight, dealing with constipation, and getting medical help for worrying symptoms are important.
Key Takeaways
- Pelvic organ prolapse is a common condition where pelvic organs drop from their normal position due to a weakened pelvic floor.
- Postpartum prolapse specifically refers to prolapse that occurs after childbirth, affecting up to 50% of women.
- Prolapse can cause uncomfortable symptoms like pelvic pressure, urinary/bowel issues, and painful sex.
- Effective treatment options include pelvic floor exercises, vaginal pessaries, and surgery in severe cases.
- Early diagnosis and management of postpartum prolapse is crucial to prevent the condition from worsening.
Understanding Postpartum Prolapse
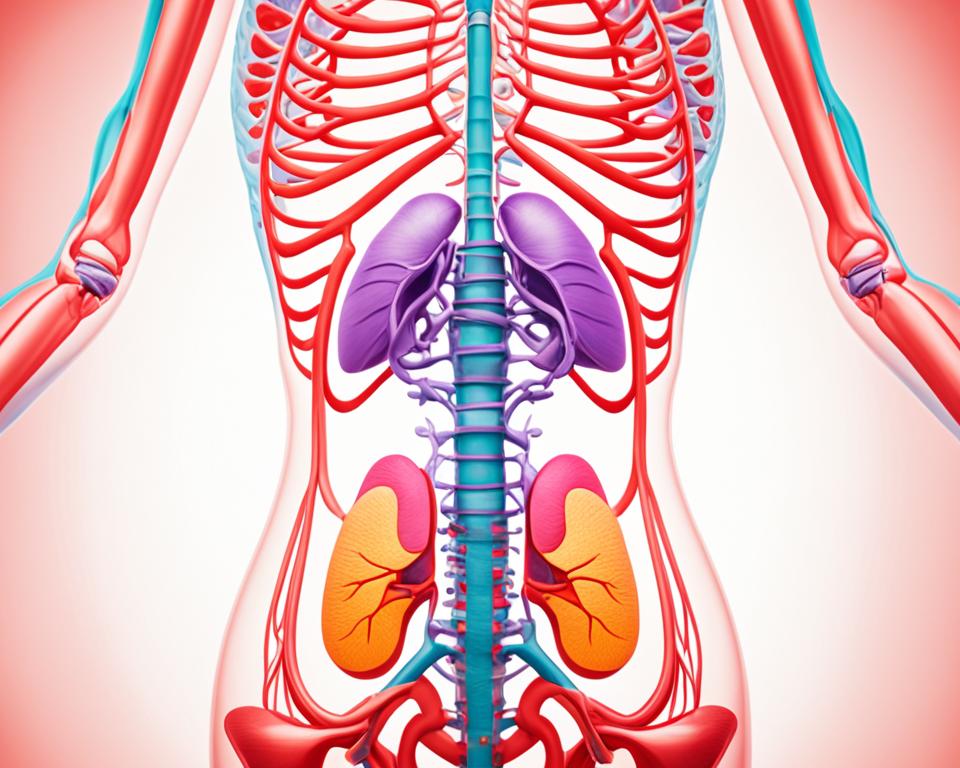
Pelvic organ prolapse occurs when organs like the bladder, uterus, or rectum move from their place. This occurs because the pelvic floor is weak. The pelvic floor is a group of muscles and tissues that hold these organs up. Giving birth, being pregnant, and other issues can make the pelvic floor weak.
What is Pelvic Organ Prolapse?
Postpartum prolapse is when this condition occurs after women have babies. During pregnancy and birth, the pelvic floor is stretched and often weakened. So, the organs may slip down.2
Causes of Postpartum Prolapse
Pregnancy and giving birth put a lot of stress on the pelvic floor. This stress can lead to postpartum prolapse.12
Risk Factors for Postpartum Prolapse
There are many things that can make postpartum prolapse more likely. These include having many children, getting older, being overweight, and suffering from constipation often. Genetics also play a role if they affect your connective tissues.12 Changing your lifestyle and working on your pelvic floor can reduce your risk.
Symptoms of Postpartum Prolapse
After giving birth, you might feel a fullness or pressure in your pelvis. It could seem like something is coming out of your vagina. You might have trouble peeing or pooping, feel constipated, have back pain, or find sex painful.3 After childbirth, feeling these mild symptoms is normal because the uterus might sag a bit.3
Common Symptoms of Pelvic Organ Prolapse
If your uterus drops more, you might see or feel a bulge in your vagina. You could feel dragging in your pelvis or, like, your bladder isn’t empty all the way. Other signs include leaking urine, pooping issues, and a sense that something is inside the vagina.3 You might also experience vaginal tissue rubbing against your clothes or experience pelvis or back pain. Sex can become uncomfortable if your vagina seems loose.3
Stages of Postpartum Prolapse
Prolapse experts divide it into four stages. Stage 1 is when the organ moves slightly into the vagina, and stage 4 is when it’s totally outside. Stages 1 and 2 involve the organ dropping but not yet reaching the opening, while stages 3 and 4 mean it’s bulging out.1 Sometimes, you won’t feel anything in the early stages. The more advanced the prolapse, the more discomfort and trouble it can cause.1
What is Postpartum Prolapse?
Definition of Postpartum Prolapse
Postpartum prolapse is a condition where pelvic organs move out of place after childbirth.4 It’s pretty common, affecting about half of all women who have given birth.1 This happens when the pelvic floor loses its strength and support during pregnancy and birth.
Postpartum Prolapse and the Pelvic Floor
The pelvic floor is like a hammock that supports organs like the bladder, uterus, and rectum.1 Without this strong support, these organs can drop and push into the vagina after giving birth.
This dropping and pushing into the vagina is what’s known as postpartum prolapse.4
Treatment Options for Postpartum Prolapse
Women with postpartum prolapse have various treatment choices. These include non-surgical options and surgical treatments. The best option depends on how severe the prolapse is, the symptoms, and the woman’s preferences.
Non-Surgical Treatments for Prolapse
In mild cases, non-surgical methods work well.4 Doing pelvic floor exercises, like Kegels, can make a big difference. They strengthen the muscles that hold up the pelvic organs. This can reduce prolapse symptoms.4 Vaginal pessaries, soft silicone devices can also help by offering support.4 Plus, making healthy lifestyle changes, such as avoiding constipation and shedding excess weight, can improve the situation.
Surgical Treatments for Prolapse
Sometimes, surgery is needed for more serious prolapse cases.4 A hysterectomy might be done to fix a prolapsed uterus. Or surgeons can use mesh to lift and support the pelvic organs.4 The choice to have surgery depends on the woman’s own health, symptoms, and goals.5 Research shows that around a third of pregnant women needing cesarean sections later had stage 2 prolapse. This hint suggests some may need more serious treatment.
It’s key for women with postpartum prolapse to collaborate with a urogynecologist or pelvic floor expert.5 Physical therapy can be part of the treatment plan. It can make symptoms better. For some, a pessary or surgery might be the answer.4 The right care and treatment can help many women effectively handle and possibly fix their postpartum prolapse. This can help them get back to living their lives fully and maintain a healthy pelvic floor.
Prevention of Postpartum Prolapse
Up to 50% of women may face postpartum prolapse after giving birth,1 but steps exist to avoid or lessen their impact. Regular pelvic floor exercises, like kegels, are valuable for muscle strength.6 Physical therapy for the pelvic floor can also teach proper muscle engagement.
Pelvic Floor Exercises
Kegel exercises are key for a strong pelvic floor and reduce prolapse risk.6 These routines are simple, done by tightening and holding the pelvic floor for a few seconds. Proper rest after giving birth and light physical activities also prevent uterine prolapse.6 It’s crucial to exercise the hip and anal muscles to keep uterine prolapse at bay in postpartum women too.6
Lifestyle Changes to Prevent Prolapse
Aside from exercise, changing habits can lower the chance of postpartum prolapse. This includes staying at a healthy weight, keeping bowel movements regular, and not doing activities that overwork the pelvic floor.3 For some, avoiding multiple births and treating chronic coughs can be necessary steps. These changes support the pelvic floor and reduce prolapse risk.3
Managing Postpartum Prolapse
There are ways for women to manage postpartum prolapse. These techniques help with the condition and its symptoms.4 They can do pelvic floor exercises and use items called vaginal pessaries for support. Changing to a healthy diet and not lifting heavy things also makes a difference.4 But, it’s very important to see a doctor. A urogynecologist or pelvic floor specialist can give you the best advice.
Coping with Prolapse Symptoms
These doctors can check the prolapse and make a plan that fits each woman’s needs.4 Acting early is crucial. Non-surgical treatment might work if it’s not too severe.1 Getting help quickly can ease symptoms and stop the prolapse from getting worse.
Seeking Medical Advice
It’s good for women to know about postpartum prolapse. This way, they can take steps to keep their pelvic floor healthy and improve life after giving birth.7
Types of Postpartum Prolapse
After childbirth, the pelvic organs might shift down, causing prolapse.4 Uterine prolapse occurs when the uterus moves down the vaginal canal or out of the vagina.
Bladder prolapse, known as cystocele, occurs when the bladder bulges into the vagina. Then there’s rectal prolapse, where the rectum slips out through the anus.4 Each type is due to a weak pelvic floor, but symptoms and treatments differ with the organ involved.1
For instance, uterine prolapse might feel like a falling sensation, while bladder prolapse might lead to trouble urinating or incontinence. Knowing this kind of prolapse is key to treating it well.
Uterine Prolapse
Uterine prolapse occurs when the uterus drops into or outside the vagina.1 It results from weakened pelvic floor muscles or structures supporting the uterus. This can make one feel a pelvic fullness or pressure and trouble with bowel or bladder control.
Bladder Prolapse
4 Bladder prolapse, or cystocele, is when the bladder bulges into the vagina. It occurs when the muscles and tissues that hold up the bladder become weak, often after pregnancy. Signs may include leaking urine, trouble peeing, and a sense of pressure in the vagina.
Rectal Prolapse
4 Rectal prolapse means the rectum pushes out through the anus. Pelvic floor weaknesses can make this happen. It can lead to feelings like something is sticking out, issues with bowel control, and sometimes, not being able to hold in stool.
Risk Factors for Postpartum Prolapse
The strains of pregnancy and childbirth, especially through the vagina, are major causes of pelvic floor weakening and prolapse.5 During these times, the muscles and tissues in the area can be harmed.5 Changes from aging and hormone shifts like in menopause also weaken the pelvic floor.3
Pregnancy and Childbirth
The impact of pregnancy and birth on the pelvic floor is significant. Studies show prolapse is more likely if labor is long, the baby is large, or if there’s assistance like forceps.5 Vaginal births can lead to prolapse more often than C-sections.5 A study discovered about a third of women in late pregnancy have stage 2 prolapse. This dropped a lot after giving birth.5
Age and Hormonal Changes
As age increases and hormones change, the pelvic floor can get weaker, especially after menopause.3 After menopause, uterine prolapse usually happens if a woman has had vaginal births.3 The effects of aging, combined with childbirth, are main causes of postpartum prolapse.
Obesity and Chronic Conditions
Being obese or having pelvic surgery before, along with chronic constipation and heavy lifting when pooping, can up the risk of prolapse.3 Family history and a lot of coughing can also lead to prolapse by putting more stress on the pelvic floor.3
Knowing about these risk factors is good for preventing or handling prolapse. Doing pelvic floor exercises and maintaining a healthy weight can help a lot.
Postpartum Prolapse Exercises
Doing specific exercises can really help with postpartum prolapse.8 Pelvic floor issues are very common after giving birth. These issues can cause pain and discomfort during sex, leaking, or a feeling of something pushing down.8
Kegel Exercises
Kegel exercises work by clenching and then releasing your pelvic floor muscles. They are key to getting better after birth. Besides kegels, other exercises like breathing and stretching can strengthen your pelvic floor.8 Doing these exercises right is important. This can lessen the chance of prolapse.
Pelvic Floor Physical Therapy
Seeing a pelvic floor physical therapist can really make a difference.8 They teach exercises that fix your tummy and build up your pelvic floor. These experts can also use special methods to make sure you’re working the right muscles. They might use equipment to check if the exercises are working.
It’s best to do these exercises with a therapist. They’ll know the best ways to help you safely.8
Combining Kegel’s work with therapy is key to your recovery.8 Postpartum products like peri bottles and Sitz baths can also speed up healing. They’re helpful for all moms, whether they had a vaginal birth or a C-section.8
Conclusion
Postpartum prolapse is common after birth. It happens when the muscles in the pelvis become weak or damaged.9 Women might feel like there’s pressure or bulging in their pelvis. They could also have trouble peeing or pooping and find sex painful.9 Thankfully, there are ways to treat and prevent this condition.
In mild cases, women can try exercise and use vaginal pessaries. Lifestyle changes also help. But for severe prolapse, surgery might be needed.9 It’s crucial to see a urogynecologistor pelvic floor specialist if you have these symptoms. Getting help early can stop the prolapse from getting worse.9
Learning about postpartum prolapse is key to taking care of your pelvic health. By working with health experts, women can overcome this issue and improve their well-being after giving birth.9 Together, they can find the best ways to treat prolapse and put women’s health first.
FAQ
What is pelvic organ prolapse?
Pelvic organ prolapse means one or more organs in the pelvis shift from their place. This shifting happens because the pelvic floor weakens. The organs include the vagina, uterus, bladder, urethra, small intestine, and rectum.
What causes postpartum prolapse?
After giving birth, the body goes through a lot. This includes weakening of the muscles and tissues that support the organs in the pelvis. This weakening leads to postpartum prolapse.
What are the symptoms of postpartum prolapse?
Feeling full in the pelvis or pressure is common. Also, you might have trouble with urination or passing stool. Pain during sex is another possible symptom.
What are the treatment options for postpartum prolapse?
Non-surgical choices for treatment include pelvic floor exercises or using vaginal pessaries. In more serious cases, surgery might be an option.
How can postpartum prolapse be prevented?
To prevent postpartum prolapse, keep a healthy weight and treat constipation. If you notice any unusual symptoms, see a doctor right away.
What are the risk factors for developing postpartum prolapse?
The risk of postpartum prolapse increases with multiple childbirths and older maternal age. It’s also linked to obesity, chronic constipation, and genetic issues with connective tissues.
What are the different types of postpartum prolapse?
You can have uterine prolapse, bladder prolapse, or rectal prolapse. Each kind affects the placement of different pelvic organs.
How can postpartum prolapse be managed?
Management includes exercises to strengthen the pelvic floor. Using pessaries, lifestyle changes, and visiting a specialist are also important steps.
What is the role of pelvic floor exercises in treating postpartum prolapse?
Kegels and other exercises can make the pelvic floor stronger. This supports the organs better and helps reduce prolapse risks and symptoms.
When should a woman seek medical care for postpartum prolapse?
If you notice any symptoms of postpartum prolapse, talk to a doctor. Early care can prevent the issue from getting worse.
Source Links
- https://rightasrain.uwmedicine.org/well/health/prolapse-after-pregnancy
- https://australianbirthstories.com/postpartum/prolapse-after-birth-understanding-the-causes-symptoms-and-treatment-options/
- https://www.mayoclinic.org/diseases-conditions/uterine-prolapse/symptoms-causes/syc-20353458
- https://www.pelvicpaindoc.com/blog/recovering-from-postpartum-prolapse/
- https://www.whattoexpect.com/first-year/postpartum-health-and-care/pelvic-organ-prolapse
- https://www.vinmec.com/en/news/health-news/obstetrics-gynecology-and-assisted-reproductive-technologies-art/prevention-of-uterine-prolapse-after-childbirth
- https://www.acog.org/womens-health/experts-and-stories/the-latest/healing-and-adjusting-after-pelvic-organ-prolapse
- https://www.whattoexpect.com/first-year/postpartum-health-and-care/postpartum-pelvic-floor-exercises
- https://www.myinnovo.com/blogs/innovo/navigating-postpartum-pelvic-organ-prolapse-effectively