Necrotic brain tissue is brain tissue that has died due to lack of blood supply, oxygen, or infection. It can cause serious complications such as stroke, abscess, or gangrene. Necrotic brain tissue cannot be reversed or healed, and it usually forms a cavity surrounded by scar tissue over time.
Necrotic Brain Tissue is our informative guide to necrotic brain tissue. In this article, we will explore the pathology, causes, and potential implications of necrotic brain tissue on overall health and well-being. Understanding this condition is crucial to providing better care and support to those affected by brain tissue necrosis
Necrotic brain tissue can be diagnosed by imaging tests such as MRI or CT scan, or by biopsy. Treatment options depend on the cause and extent of the necrosis, but they may include surgery, antibiotics, or anticoagulants.
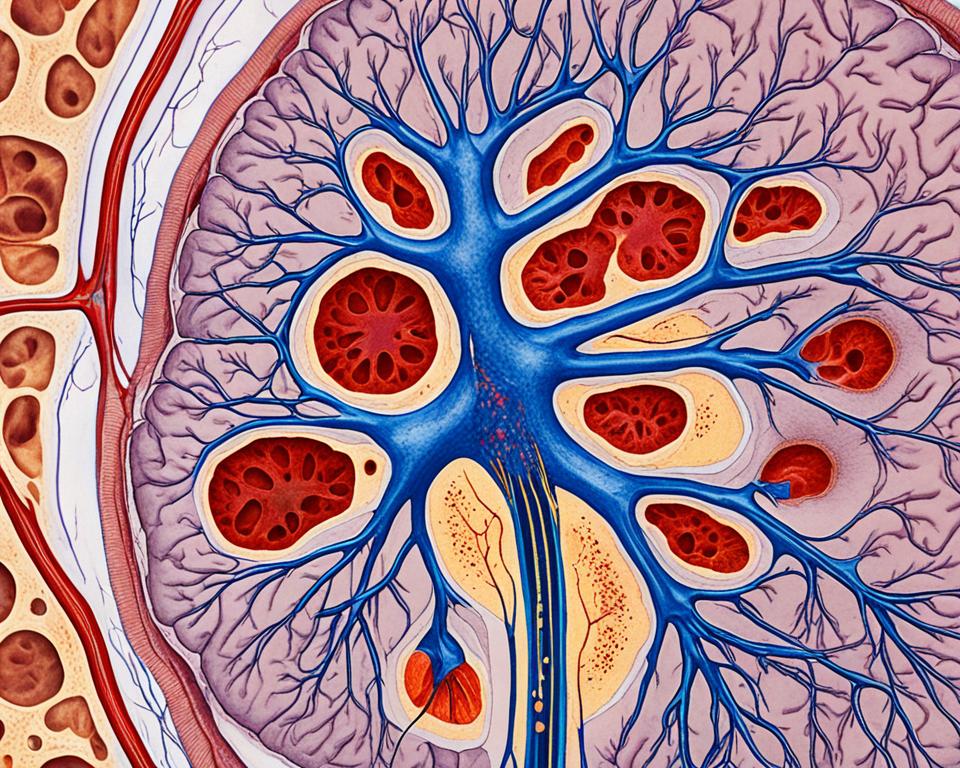
Table of Contents
ToggleKey Takeaways
- Necrotic brain tissue is a condition characterized by the death of brain cells, resulting in impaired brain function.
- Brain tissue necrosis can be caused by external factors such as trauma or internal factors such as underlying health conditions.
- The diagnosis of necrotic brain tissue involves imaging techniques like MRI and clinical assessments.
- Necrotic brain tissue can have significant implications for cognitive function, emotional well-being, and physical health.
- Understanding necrotic brain tissue enables us to empathize with affected individuals and work towards improved care and support.
Understanding Necrotic Brain Tissue
Necrotic brain tissue refers to the death or decay of brain cells due to a lack of oxygen supply. The condition, known as brain tissue necrosis, can have significant implications for overall brain function and health.
The process of brain tissue necrosis typically occurs when there is a disruption in blood flow to the brain, leading to ischemia. Without sufficient oxygen and nutrients, the affected brain cells begin to deteriorate and ultimately die. This can result from various factors, including:
- Stroke
- Head trauma
- Tumors
- Infections
- Severe hypoxia
As necrotic brain tissue progresses, it can lead to significant consequences for an individual’s cognitive function and overall well-being. The extent of these consequences depends on the location and severity of the brain tissue necrosis.
“Necrotic brain tissue can have a profound impact on an individual’s quality of life, affecting their ability to think, speak, and perform everyday tasks,” said Dr. Emma Johnson, a neurologist at the XYZ Medical Center.
Research indicates that necrotic brain tissue can result in various cognitive impairments, such as memory loss, difficulty concentrating, and decreased problem-solving abilities. It can also impact motor skills, coordination, and emotional regulation.
Potential Consequences of Necrotic Brain Tissue:
| Consequences | Description |
|---|---|
| Cognitive Impairment | Memory loss, difficulty concentrating, decreased problem-solving abilities. |
| Motor Dysfunction | Impaired coordination, reduced muscle control, difficulties with speech and swallowing. |
| Emotional Instability | Mood swings, depression, anxiety, irritability. |
| Functional Limitations | Difficulties with self-care, impaired ability to perform daily activities. |
It is essential to seek prompt medical attention if necrotic brain tissue is suspected. Diagnosis typically involves a combination of medical history, neurological examination, and imaging techniques such as MRI and CT scans to assess the extent of brain tissue necrosis.
While treatment options for necrotic brain tissue are limited, medical professionals focus on managing the underlying cause, preventing further damage, and providing supportive care to improve an individual’s quality of life.
By understanding necrotic brain tissue and its potential consequences, we can raise awareness and contribute to the development of better preventive strategies and interventions to support individuals affected by this condition.
Causes and Risk Factors of Necrotic Brain Tissue
To understand the occurrence of necrotic cerebral tissue, it is crucial to explore the various causes and risk factors that contribute to brain tissue damage and cerebral tissue injury.
External Factors
Brain tissue damage can occur as a result of traumatic events and injuries, which can lead to cerebral tissue necrosis. These external factors may include:
- Head trauma caused by accidents or falls
- Cerebral ischemia due to strokes
- Exposure to toxins that target the brain
Internal Factors
In addition to external causes, several underlying health conditions can increase the risk of developing necrotic cerebral tissue. Some internal factors include:
- Neurodegenerative disorders, such as Alzheimer’s disease and Parkinson’s disease
- Brain tumors and malignancies
- Autoimmune disorders, like multiple sclerosis
- Infections that affect the brain, such as meningitis or encephalitis
It’s important to note that these causes and risk factors can vary from person to person. Consulting a healthcare professional is essential to receive accurate diagnosis and appropriate treatment.
Understanding the causes and risk factors of necrotic cerebral tissue is crucial for early detection, prevention, and effective treatment. It allows healthcare providers to address these underlying factors and implement suitable interventions to minimize brain tissue damage and improve overall health outcomes.
Causal Factors and Risk Factors of Necrotic Brain Tissue
| Causal Factors | Risk Factors |
|---|---|
| Head trauma | Neurodegenerative disorders |
| Cerebral ischemia | Brain tumors and malignancies |
| Toxin exposure | Autoimmune disorders |
| Infections affecting the brain |
Pathology and Diagnosis of Necrotic Brain Tissue
In this section, we will explore the fascinating pathology of necrotic brain tissue, shedding light on its progressive nature and the diagnostic methods used to identify necrosis of the brain.
Necrotic brain tissue refers to the degeneration and death of brain cells due to various factors, including trauma, infections, and inadequate blood supply. The decay of brain tissue can have significant consequences for overall brain function and can be a challenging condition to diagnose.
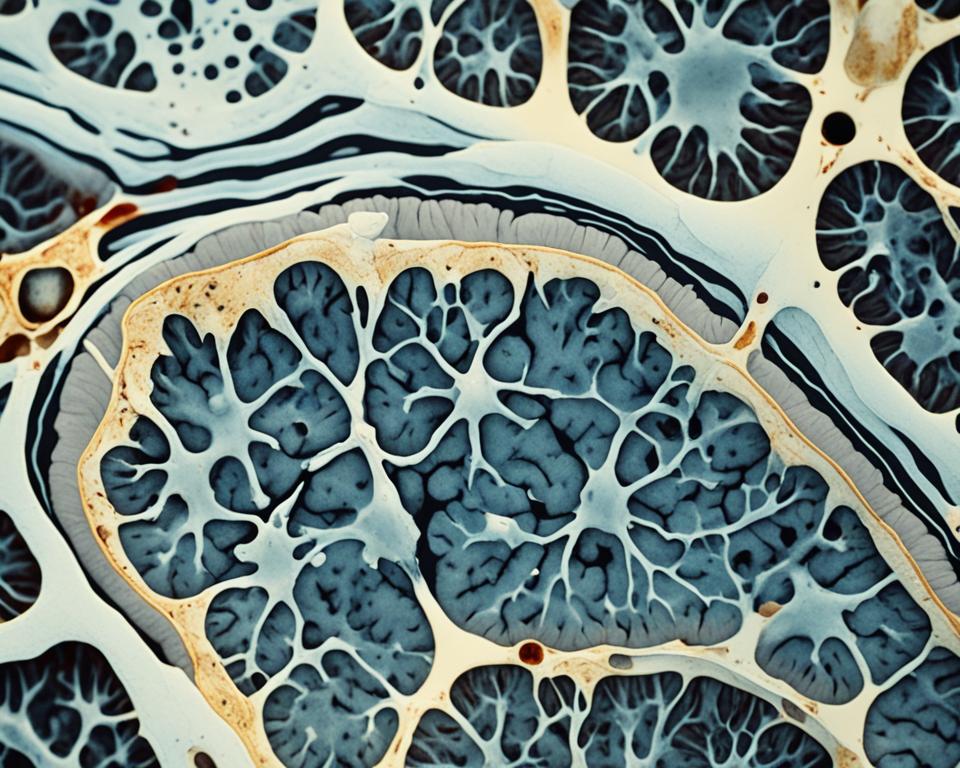
One of the primary diagnostic tools used to identify necrotic brain tissue is magnetic resonance imaging (MRI). This non-invasive imaging technique provides detailed images of the brain, allowing healthcare professionals to visualize any abnormalities or areas of tissue decay.
Additionally, other clinical assessments may be utilized to determine the presence of necrosis in the brain. These assessments can include neurological examinations, cognitive tests, and laboratory tests to evaluate specific biomarkers associated with necrotic brain tissue.
Ultimately, an accurate diagnosis is vital for the appropriate management and treatment of individuals with necrosis of the brain. The information gathered from these diagnostic methods helps healthcare professionals develop a comprehensive understanding of the extent of brain tissue decay and its impact on an individual’s health.
Diagnostic Methods for Necrotic Brain Tissue
The diagnostic methods for necrotic brain tissue primarily include:
- Magnetic Resonance Imaging (MRI)
- Neurological examinations
- Cognitive tests
- Laboratory tests to evaluate biomarkers
By utilizing these diagnostic techniques, healthcare professionals can accurately identify and assess the presence of necrosis in the brain, enabling them to provide the most effective treatment and care for their patients.
| Diagnostic Method | Description |
|---|---|
| Magnetic Resonance Imaging (MRI) | Non-invasive imaging technique that provides detailed images of the brain, allowing visualization of abnormalities and areas of tissue decay. |
| Neurological examinations | Assessment of neurological function to evaluate brain health and identify any indications of necrotic brain tissue. |
| Cognitive tests | Evaluation of cognitive function to assess the impact of necrotic brain tissue on cognitive abilities, such as memory, attention, and language skills. |
| Laboratory tests | Testing of specific biomarkers is associated with necrotic brain tissue, providing additional insights into the condition. |
Through the combined use of these diagnostic methods, healthcare professionals can gain a comprehensive understanding of necrotic brain tissue, its progression, and the potential impact on an individual’s overall health and well-being.
Implications of Necrotic Brain Tissues on Health
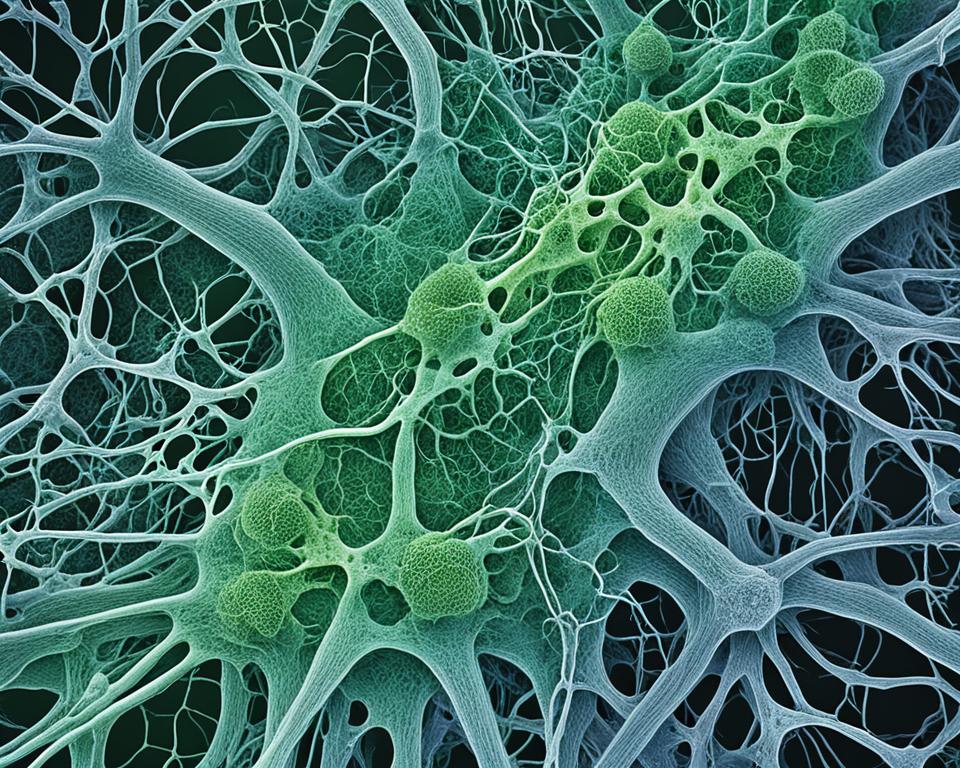
Necrotic brain tissue can have significant implications for an individual’s overall health and well-being. The death of brain tissue, medically known as necrosis, can lead to a range of cognitive, emotional, and physical challenges. Understanding these implications is crucial for providing appropriate care and support to those affected.
The Impact on Cognitive Function
When brain tissue undergoes necrosis, it can result in the disruption of crucial neuronal pathways and communication within the brain. This can lead to cognitive impairments such as memory loss, difficulty concentrating, and problems with language and decision-making. Individuals may also experience changes in perception and reasoning abilities, making everyday tasks more challenging.
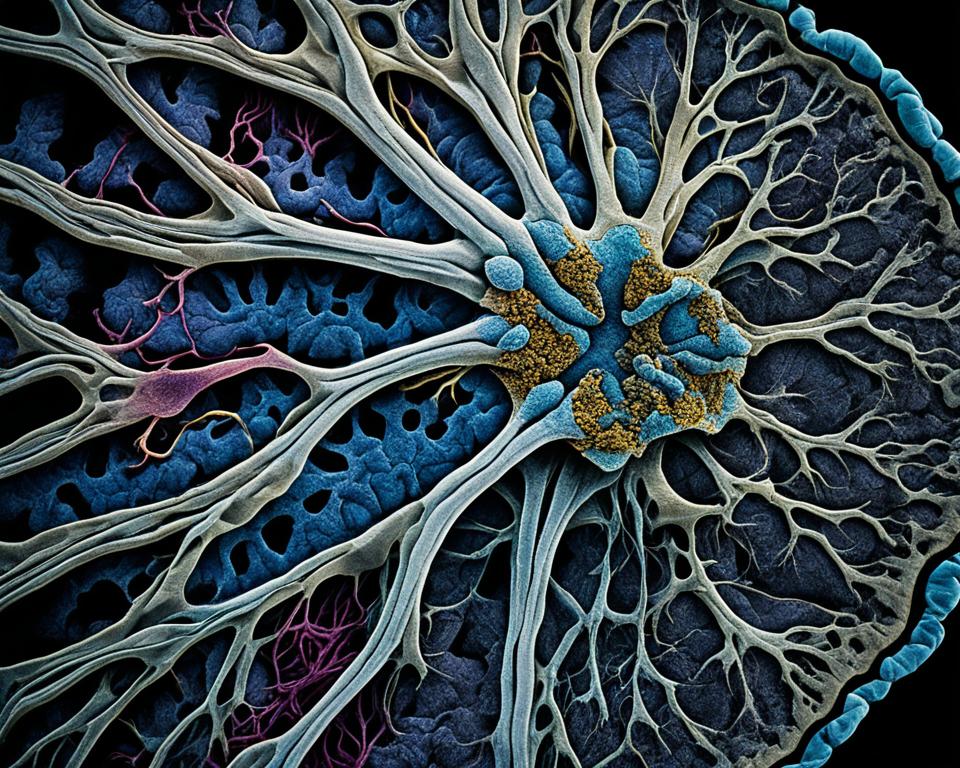
The Effects on Emotional Well-Being
The death of brain tissue can also impact a person’s emotional well-being. Areas of the brain affected by necrosis are often responsible for regulating emotions, mood, and behavior. As a result, individuals may experience mood swings, heightened anxiety, depression, and a decrease in their overall emotional resilience. Coping with these emotional changes can be a significant challenge for both the individual and their loved ones.
Physical Consequences
The consequences of necrotic brain tissue extend beyond cognitive and emotional effects. The brain is responsible for controlling the body’s physical functions, and when brain tissue dies, it can lead to various physical impairments. These may include difficulties with motor skills, coordination, balance, and even paralysis in some cases. The physical consequences of brain tissue death can significantly impact an individual’s quality of life and independence.
“The death of brain tissue can have profound implications for an individual’s cognitive function, emotional well-being, and physical health. Understanding these implications is vital for providing comprehensive care and support to those living with necrotic brain tissue.” – Dr. Sarah Thompson
To better comprehend the implications of necrotic brain tissue on health, it is essential to consider the interconnectedness of cognitive, emotional, and physical well-being. Addressing these implications requires a multidisciplinary approach involving healthcare professionals, therapists, and support networks.
By raising awareness and promoting research into necrotic brain tissue, we can strive for improved understanding, early detection, and more effective treatments for those impacted by this challenging condition.
Conclusion
In conclusion, this comprehensive guide has provided valuable insights into the complex nature of necrotic brain tissue, shedding light on its pathology and implications for overall health. By deepening our understanding of the causes, risk factors, diagnosis, and impact associated with necrotic brain tissue, we are better equipped to offer empathy, care, and support to individuals affected by this condition.
Through this journey, we have learned that necrotic brain tissue can arise from various external factors, such as trauma and injury, as well as internal factors like underlying health conditions. Diagnosis methods, including advanced imaging techniques like MRI, play a crucial role in identifying brain tissue necrosis and guiding treatment decisions.
Moreover, the guide has emphasized the significance of necrotic brain tissue on cognitive function, emotional well-being, and physical health. Individuals grappling with brain tissue death face unique challenges that require a multi-faceted approach to care, involving medical interventions, rehabilitation, emotional support, and lifestyle adjustments. By fostering a holistic understanding of this condition, we can pave the way for improved care and support systems.
In conclusion, this guide serves as a valuable resource for individuals seeking knowledge about necrotic brain tissue, healthcare professionals involved in its diagnosis and treatment, and society at large. By continuing to raise awareness, conduct research, and promote empathy, we can strive towards enhancing the quality of life for those affected by necrotic brain tissue.
FAQ
What is necrotic brain tissue?
Necrotic brain tissue refers to the death or decay of cerebral tissue. It occurs when brain cells experience a lack of blood flow or oxygen, leading to irreversible damage and ultimate demise.
What causes necrotic brain tissue?
Necrotic brain tissue can be caused by various factors, including traumatic brain injuries, strokes, infections, tumors, and certain medical conditions such as cerebral infarction. These events can disrupt the blood supply to the brain, resulting in tissue death.
How is necrotic brain tissue diagnosed?
The diagnosis of necrotic brain tissue typically involves a combination of imaging techniques, such as MRI (Magnetic Resonance Imaging), CT (Computed Tomography), and PET (Positron Emission Tomography) scans. Clinical assessments, medical history evaluation, and neurological examinations may also be done to confirm the presence of necrosis in the brain tissue.
What are the potential implications of necrotic brain tissue on health?
Necrotic brain tissue can have significant implications on an individual’s health and well-being. It can lead to various cognitive impairments, including memory loss, difficulty with speech and language, and problems with executive functions. Emotional changes, physical disabilities, and even coma or death can also occur depending on the location and extent of the tissue necrosis.
Is there any treatment available for necrotic brain tissue?
Treatment options for necrotic brain tissue depend on the underlying cause and severity of the condition. In some cases, emergency interventions, such as surgery or clot-dissolving medications, may be necessary. Rehabilitation therapies, including physical, occupational, and speech therapies, are often employed to support recovery and maximize quality of life.
Can necrotic brain tissue be prevented?
While it may not always be possible to prevent necrotic brain tissue in every circumstance, certain lifestyle choices can reduce the risk. These include maintaining a healthy diet, exercising regularly, managing chronic health conditions, and avoiding behaviors that may lead to head injuries or strokes. Early detection and prompt medical intervention are also crucial in minimizing the impact of necrosis on the brain tissue.
Can necrotic brain tissue be reversed?
Unfortunately, necrotic brain tissue cannot be reversed or regenerated. Once brain cells are damaged or die, they cannot be fully restored. However, therapy and rehabilitation programs can help individuals cope with the consequences of necrosis and regain as much function as possible by promoting neural plasticity and adaptation.

Comments are closed.