HIV rash is a dermatological manifestation generally discovered in individuals infected with the human immunodeficiency virus (HIV).
It serves as an important clinical indicator, frequently performing at some point in the intense section of HIV infection.
Expertise in traits, identity techniques, and treatment options for HIV warts is important for healthcare experts and people living with HIV/AIDS.
In this comprehensive guide, we will explore intricate information on HIV rash, incorporating superior study findings, and medical insights to offer complete expertise in this situation.
Table of Contents
ToggleWhat is HIV Rash?
HIV rash is a non-specific dermatological manifestation related to HIV contamination.
It normally acts as a maculopapular rash characterized by the aid of pink or purple lesions on the pores and skin.
The rash can also vary in severity, distribution, and morphology, ranging from discrete papules to confluent plaques.
While HIV warts predominantly affect the trunk and proximal extremities, they may also involve the face, hands, and soles.
The pathogenesis of HIV warts is multifactorial, related to viral replication, immune dysregulation, and inflammatory mediators.
Histopathological exam famous capabilities constant with a hypersensitivity reaction, vasculitis, or infectious etiology, highlighting the complexity of HIV-related dermatoses.
Figuring Out HIV Rash:
Accurate identification of HIV requires a complete evaluation of scientific features, patient records, and laboratory investigations.
Clinically, HIV warts provides a polymorphous eruption characterized via erythematous papules, macules, or plaques.
The lesions may be pruritic or asymptomatic, evolving over days to weeks.
Extensively, HIV rash is regularly followed with the aid of systemic signs and symptoms consisting of fever, malaise, and lymphadenopathy, reflecting the underlying viral replication and immune response.
The thermoscopic exam may display unique patterns, including dotted vessels, scale, and pigmentary changes, aiding in the differential diagnosis of HIV-related dermatoses.
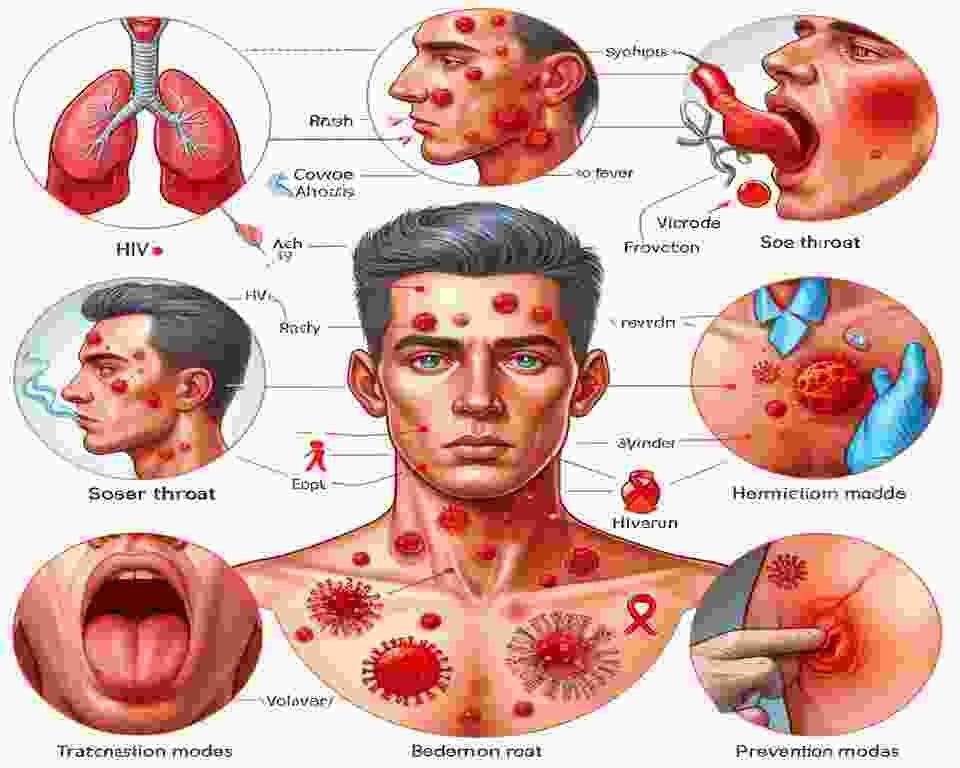
HIV Rash Pictures:
Visual documentation of HIV rashes performs a pivotal role in medical schooling, diagnostic accuracy, and affected personal counseling.
A curated collection of HIV warts images showcases the rash’s numerous scientific displays and temporal evolution.
From conventional maculopapular eruptions to abnormal editions consisting of eosinophilic pustular folliculitis and acute generalized exanthemata’s pustulosis, those images provide worthwhile insights into the morphological spectrum of HIV rashes.
Additionally, comparative analysis with other dermatological situations, such as drug reactions, viral exanthems, and autoimmune problems, enhances diagnostic precision and therapeutic choice-making.
Location: Face and Others:
The predilection of HIV warts for precise anatomical websites, which include the face, displays underlying pathophysiological mechanisms and host elements.
Facial involvement in HIV may additionally happen as discrete papules, erythematous patches, or confluent plaques, often sparing the nasolabial folds and periorbital regions.
The distribution of HIV warts in the face correlates with regional lymphatic drainage patterns and immune mobile infiltration, highlighting the complicated interplay between viral replication and host immune response.
Moreover, extracutaneous manifestations of HIV infection, such as oral candidiasis and herpes zoster, may additionally coexist with facial rash, necessitating a holistic approach to affected person evaluation and control.

Timeline of HIV Rash:
The temporal evolution of HIV rash parallels the dynamic path of HIV contamination, reflecting versions in viral load, immune reputation, and treatment reaction.
Acute HIV warts generally takes place during the seroconversion duration, 2-6 weeks following number one infection, coinciding with height viremia and CD4+ T-cellular depletion.
The rash may additionally persist for several weeks before resolving spontaneously or evolving into continual dermatoses, such as seborrheic dermatitis or pruritic popular eruption.
Notably, the absence of rashes at some point of acute HIV contamination no longer excludes HIV seroconversion, emphasizing the significance of complete diagnostic checking out and clinical tracking.
Acute HIV Rash:
Acute HIV warts represent an indicator characteristic of number one HIV contamination, heralding the onset of systemic viral replication and immune activation.
Clinically, acute HIV rash occurs as a diffuse, erythematous eruption affecting the trunk, extremities, and face.
The rash is regularly followed by using constitutional signs and symptoms such as fever, sore throat, myalgias, and headaches, mimicking infectious mononucleosis and viral exanthems.
Early recognition of acute HIV warts is vital for timely analysis and initiation of antiretroviral therapy (artwork), which can attenuate viral replication, hold immune features, and mitigate long-term period complications of HIV infection.
Remedy Alternatives:
The remedy for HIV incorporates a multimodal technique aimed at symptom alleviation, viral suppression, and immune reconstitution.
Pharmacological interventions can also consist of:
Antiretroviral Therapy (Art):
Suppresses viral replication, reduces HIV-associated infection, and promotes immune reconstitution.
Topical Corticosteroids:
Alleviate pruritus and inflammation, especially in localized or moderate cases of HIV rashes.
Antihistamines:
Offer symptomatic remedies for itching and pain, enhancing the affected person’s consolation and adherence to treatment.
Systemic Agents:
Reserved for intense or refractory instances of HIV warts, this includes systemic corticosteroids, immunomodulators, and antiviral medicinal drugs.
Further to pharmacotherapy, adjunctive measures along with emollients, phototherapy, and lifestyle modifications may supplement the management of HIV warts.
Patient schooling and counseling are paramount, emphasizing the importance of medication adherence, regular follow-up, and early detection of treatment-associated destructive activities.
Collaborative care involving dermatologists, infectious disease experts, and allied healthcare experts optimizes affected person effects and fosters holistic control of HIV-related dermatoses.
Prevention and Headaches:
Stopping HIV warts necessitates a complete technique for HIV prevention, which includes:
HIV Testing and Counseling:
Encourages early detection of HIV contamination, enables linkage to care, and mitigates the threat of HIV-related headaches.
Safer Intercourse Practices:
Promotes condom use, pre-publicity prophylaxis (PrEP), and danger reduction strategies to save you from HIV transmission.
Harm Reduction Offerings:
Presents access to sterile injection gadgets, opioid substitution therapy, and overdose prevention programs to reduce HIV risk amongst people who inject tablets (PWID).
Network-Based Interventions:
Engage key populations, including men who have intercourse with men (MSM), transgender individuals, intercourse people, and those living with HIV/AIDS (PLWHA), in HIV prevention efforts tailor-made to their precise desires and vulnerabilities.
Headaches from the HIV warts can also include secondary infections, immune-mediated dermatoses, and psychosocial sequelae.
Prompt reputation and management of headaches, along with cellulitis, eczema herpeticum, and immune reconstitution inflammatory syndrome (IRIS), are critical to decreasing morbidity and mortality amongst affected people.
Long-term period tracking and supportive care, inclusive of intellectual fitness offerings, social support networks, and adherence counseling, optimizes the best of existence for PLWHA laid low with HIV warts and its sequelae.

Conclusion:
In conclusion, HIV rash represents a multifaceted dermatological manifestation of HIV contamination, reflecting the dynamic interaction between viral pathogenesis and host immune response.
Superior research findings and scientific insights have elucidated the pathophysiology, analysis, and management of HIV rashes, paving the manner for customized healing interventions and advanced affected person results.
With the aid of embracing a holistic technique for HIV care, encompassing early diagnosis
Frequently Requested Questions Approximately HIV Rash:
1. What causes HIV rash?
HIV rash is on the whole attributed to the immune response in opposition to the human immunodeficiency virus (HIV) itself.
It could additionally result from opportunistic infections, damaging reactions to medicines, or immune reconstitution inflammatory syndrome (IRIS) following initiation of antiretroviral remedy (art).
2. Is HIV rash an early sign of HIV infection?
Sure, HIV rash may be one of the early signs and symptoms of HIV contamination, generally going on at some stage in the intense phase of the disease.
It frequently manifests within 2-6 weeks following exposure to the virus, coinciding with seroconversion and heightened viremia.
3. How was the HIV rash diagnosed?
Diagnosis of HIV rash involves an intensive medical evaluation, which includes assessment of clinical records, physical exams, and laboratory testing.
A dermatological exam and skin biopsy may be carried out to confirm the analysis and rule out different dermatoses.
4. Can an HIV rash be itchy?
Sure, HIV rashes may be pruritic (itchy), even though not all individuals experience itching. Pruritus may also vary in depth and may worsen over the course of intervals of extended viral replication or immune activation.
5. What are the remedy options for HIV rash?
Remedy of HIV rash makes it a specialty of symptom remedy, viral suppression, and immune reconstitution.
Pharmacological interventions may consist of antiretroviral remedies (artwork), topical corticosteroids, antihistamines, and systemic dealers.
Adjunctive measures together with emollients, phototherapy, and way-of-life modifications will also be encouraged.
6. How long does HIV rash ultimate?
The duration of the HIV rash varies depending on character elements along with immune popularity, treatment adherence, and underlying comorbidities.
In maximum instances, HIV rash resolves spontaneously within a few weeks, although continual or recurrent cases may require ongoing control.
7. Can an HIV rash appear on the face?
Yes, HIV rash can happen on the face, offering pink patches, papules, or plaques.
Facial involvement may additionally arise simultaneously with trunk and limb rash or as a remote manifestation of HIV-related dermatoses.
8. Is HIV rash contagious?
No, the HIV rash itself is not contagious as it is a manifestation of the underlying HIV contamination.
However, certain opportunistic infections or coexisting dermatological situations related to HIV rash can be contagious, necessitating appropriate precautions and treatment.
9. How can an HIV rash be averted?
Prevention of HIV rash entails early diagnosis and remedy of HIV infection, adherence to antiretroviral remedy (artwork), and adoption of safer sex practices to reduce the threat of transmission.
Preserving good hygiene, fending off irritants, and minimizing publicity for ability allergens may also assist in saving you from exacerbations of HIV rash.
10. When need to seek clinical interest for HIV rash?
It’s miles recommended to search for scientific interest in case you experience persistent or extreme symptoms of HIV rash, which include tremendous rash, fever, swelling, or issue respiration.
Activating evaluations using a healthcare expert can facilitate timely analysis and control of HIV-associated dermatoses and associated complications.
